
People have turned to calcium acetate for centuries, though it’s easy to forget how expansive its journey has been since its first discoveries. In the 19th century, chemists noticed the reaction between calcium carbonate and acetic acid, quickly finding applications in medicine and industry. Over time, industries expanded, and so did the demand for simple, reliable compounds to control phosphorus, balance chemical reactions, and offer food preservation solutions. My experience working in pharma labs often brought out the enduring place of calcium acetate alongside many other old but reliable substances. This sort of compound’s blend of accessibility and effectiveness keeps it relevant despite decades of innovation.
Calcium acetate shows up most often as a white, odorless powder or granular substance. Its use spans pharmaceutical, food, water treatment, and industrial sectors. In the pharmaceutical industry, many appreciate it as a phosphate binder for people with advanced kidney disease. Food manufacturers rely on its role as a preservative and acidity regulator. Municipalities use it to treat water, controlling heavy metals and phosphates. My own work in quality control labs hammered home how product consistency is vital. If the acetate melts too easily or clumps, processing gets complicated, so manufacturers pay sharp attention to particle size and moisture control from batch to batch.
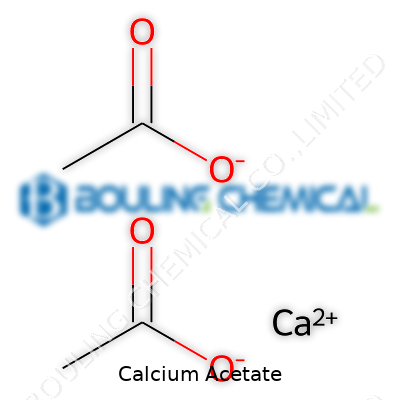
Calcium acetate stands out due to its chemical formula Ca(C2H3O2)2, with a molar mass of 158.17 g/mol. The powder dissolves readily in water, and its solubility increases in warm or hot water, but one rarely sees it dissolve in alcohol. The solution is slightly alkaline, making it fit for applications where controlling pH in manufacturing or in biological reactions is essential. At around 160°C, calcium acetate decomposes, releasing acetic acid vapors and leaving behind calcium carbonate. Working in labs, managing humidity has always seemed essential with this material since its hygroscopic nature—it tends to draw moisture from the air. The feel and appearance can shift dramatically if left out of sealed containers for even a short time, and that’s often overlooked outside the lab.
Technical specifications for calcium acetate cover purity, appearance, particle size, and water content. Pharmaceutical grades must meet strict pharmacopoeial benchmarks, maintaining at least 99% purity and tight limits on heavy metals and microbiological contamination. Labels display batch numbers, production dates, expiry, grade, and handling precautions. Over the years, I’ve seen quality assurance teams scrutinize these certificates of analysis, knowing that missed details could affect patient safety or compromise entire food batches. Those documentation requirements help trace problems back to the source if quality issues arise, turning what seems like paperwork into a vital step for consumer trust and regulatory compliance.
Manufacturers prepare calcium acetate by reacting calcium carbonate or calcium hydroxide with acetic acid. The process is straightforward, but controlling temperature, concentration, and mixing speeds tightens yields and keeps impurities out. After filtration and drying, the end product is milled or granulated for customer needs. Sometimes, calcium acetate arises as a by-product from other syntheses, but high-purity lots used in the medical field don’t cut corners. I have seen firsthand how meticulous equipment cleaning and fresh solvent batches keep contamination at bay, an aspect that lower-tier suppliers may ignore, and the difference shows.
Calcium acetate participates in a string of valuable reactions. Adding it to sulfates leads to precipitation of calcium sulfate. Exposure to oxalates generates solid calcium oxalate, which might show up in laboratory tests. It reacts with strong mineral acids to liberate acetic acid again. Its role in the textile industry and in certain organic syntheses owes much to these mild but reliable chemical properties. Modifications tend to focus on tweaking particle shape or granule size for specific batch processes in manufacturing. Laboratory people, including myself, keep a bottle on hand for quick pH adjustments or for making simple calibration mixes, enjoying the predictability of its reactions.
Calcium acetate goes by plenty of names depending on context. Chemists might say acetic acid calcium salt, and pharmacists may reference PhosLo, a popular prescription packet. Food labels sometimes list E263. Differences in labeling add to confusion, especially in global supply chains, and I remember more than one procurement mix-up caused by such ambiguities. Every experienced buyer keeps a detailed checklist for accurate sourcing, cross-referencing Latin and trade names.
Calcium acetate rates as relatively low toxicity, but dust and mishandling present real hazards. Inhalation or direct contact can irritate eyes and skin, leading companies to enforce firm use of gloves, goggles, and dust masks. Safety Data Sheets, updated often, walk end users through storage and spill procedures. In my time training staff, I learned how quickly people cut corners if they feel safe with a "benign" compound—complacency causes more accidents than exotic reagents. Facilities also set rules about food separation and locked chemical storage, building layers of protection into everyday handling routines.
Hospitals prescribe calcium acetate to patients dealing with hyperphosphatemia from chronic kidney disease. Food companies add it to bread and dairy for mold protection and acid balance. The water industry uses it to trap phosphates or tone down certain heavy metals. Some niche tech sectors draw on it in building anti-corrosive materials or specialty cements. My involvement in both pharmaceutical and food R&D always brought me back to the balancing act between cost, regulatory hurdles, and assured outcomes—which can shift drastically as regulations tighten.
Recent research centers on fine-tuning the release of calcium ions for improved medical outcomes or on blending calcium acetate into new materials for environmental remediation. Analysts in university chemistry labs study its role in biosorption of heavy metals and phosphorus from waste streams. Several times, grant applications landed on my desk focused on "green chemistry" angles—finding ways to recycle process streams and slash carbon footprints. The progress may look slow, but each step improves sustainability and opens new markets.
Published studies hold calcium acetate to a strict standard. Doses used clinically rarely drive serious side effects, but misuse—overdose or underlying health problems can tip the scales, leading to hypercalcemia. Animal studies support its low acute toxicity, but chronic exposure data remains sparse, so medical workers rely on careful patient monitoring. As someone once tasked with reviewing adverse event reports, I noticed that most issues sprang not from the compound itself, but from lack of coordination across pharmacy, nursing, and lab staff.
The market for calcium acetate remains strong, especially with kidney-related diseases appearing on the rise and food manufacturers seeking tried-and-true preservatives. Environmental interest grows as researchers look to trap phosphates in water and soil. Tech sectors also hunt for stable low-cost additives for novel composites and batteries. Each application brings new regulations to navigate, so robust supply chains and scrupulous documentation will remain essential. In my work, following both regulatory shifts and R&D projects has proved key to anticipating how even familiar compounds like calcium acetate get used in tomorrow’s world.
Every time you walk into a pharmacy or enjoy a bite of processed cheese, you run into things you usually don’t think much about. Calcium acetate is one of those invisible helpers, showing up in places you’d never expect unless you start looking at those tiny ingredient lists or dig into patient medication leaflets. I can’t count the number of times I’ve heard questions about odd chemical names from family or friends managing kidney problems. So, I took some time to really dive into what calcium acetate does for folks in real life—not just what it says on a medical chart or food label.
People who live with chronic kidney disease face a set of unique challenges. Healthy kidneys act like powerful filters, clearing extra phosphorus from the body. But when kidneys struggle, phosphorus builds up, and that starts a downward spiral. Bones can get weak, blood vessels stiffen, hearts work harder—because high phosphorus affects more than just lab results. Calcium acetate gets handed out as a phosphate binder. It "grabs" phosphorus from food in the stomach and keeps it from slipping into the bloodstream. Hospitals and clinics rely on it because its results have stood the test of time. Fewer complications, lower rates of dangerous deposits in soft tissue, and most patients seem to tolerate it pretty well compared to harsher alternatives.
Most folks don’t realize that calcium acetate also shows up in food production. It helps stop foods from getting mushy by stabilizing textures. Some bakers use it to prevent bread and pastries from molding too early, so less goes to waste. And the food-grade stuff acts as a firming agent that helps fruits and veggies stay crisp longer on store shelves. I’ve looked through the back of restaurant kitchens and seen the way a box of calcium acetate powder finds its way next to the flour and baking soda. That little scoop might keep your salad bar tomatoes from turning into tasteless slush before lunchtime ends.
Beyond food and medicine, students run into calcium acetate in every chemistry class that whips up a classic demonstration. Mix it with ethanol, and you get what’s known as “solid alcohol”—a safe, slow-burning fuel teachers love to use because it’s less likely to get out of control. I’ve seen construction workers take advantage of its knack for binding things together, especially when stabilizing soil for foundations in areas with tricky groundwater. Each industry picks it up for its own jobs, yet rarely do everyday people hear that name unless they’re knee-deep in a project or wrestling with tough health decisions.
The FDA called calcium acetate “generally recognized as safe” for food uses, but just like any chemical, using too much comes with risks. Overdoing it in supplements or medication can spike calcium levels, and then people run into other troubles. In my own experience, pharmacists and doctors have to carefully explain dosing changes, especially for patients taking multiple phosphate binders. Families need honest, clear conversations about reading labels or how to safely store powders and tablets around curious kids.
Medical researchers keep searching for ways to control phosphorus without causing side effects. Plant-based diets, careful monitoring of calcium intake, and newer binders made from polymers or iron show some promise. But until a breakthrough lands—and gets proven over years—calcium acetate fills jobs no flashy alternative has pushed aside. It’s one of those helpers that makes life a little safer and tastier, even if almost nobody notices.
Calcium acetate offers real help to people facing chronic kidney disease, especially for those looking to keep phosphate levels in check. My grandmother took it for years. She used to say it was “one of those medicines you only realize you need when you stop.” The routine made all the difference—whether at home or eating out, she knew it worked best with food, never on an empty stomach.
Calcium acetate doesn’t just block phosphorus by magic; it grabs on as food digests, forming non-absorbable compounds. Skipping a meal or taking it without food weakens its effect, so doctors stick to recommending it alongside every main meal. Simple meals, snacks, whatever—add the dose as soon as you start eating.
Mistakes happen, pills get forgotten, especially if the day packs in too much stress or routine shifts. Some folks try to “catch up” and double up at the next meal. This causes more harm than help. It can push calcium into risky levels, raising the chance for headaches, stomach pain, or even changes in heart rhythm. Instead, just take the next dose as soon as the next meal begins. No doubling, no guesswork. Health relies on consistency, not shortcuts.
Calcium acetate brings real benefits, but the body speaks up if things go wrong. Constipation is a common complaint, which doctors often address by suggesting more fiber or a gentle laxative. Too much calcium shows up in tests as hypercalcemia. Symptoms might include confusion, muscle weakness, or tiredness. Hospitals track these things carefully, but you have to speak up if something feels off. Reporting symptoms early allows adjustments, preventing worse problems.
Some medicines and vitamins clash with calcium acetate. Too much vitamin D or over-the-counter calcium supplements ramp up calcium even further, which throws off the balance doctors work so hard to set. Thyroid medicine is a unique case; calcium acetate can stop it from absorbing right. Taking thyroid medicine a few hours apart from calcium acetate usually keeps both working. Talking through the full medicine and supplement list with a trusted pharmacist or doctor gives the clearest path forward.
Routine makes the difference. Pillboxes, alerts on a smartphone, or notes on the kitchen table—no one method works for everyone. I learned from nurses in dialysis units: habits become lifelines once they’re built up. For people newly diagnosed, this takes time and patience. Family and friends can help. A support system keeps the cracks small.
Doctors adjust calcium acetate doses based on regular blood work. Improving diet by cutting down on processed foods—especially those loaded with phosphate additives—lightens the load on medicine. Every hospital I’ve visited makes food education part of the plan. Registered dietitians provide tips low on jargon and high on practical advice: label reading, meal swaps, what to buy at the market. These steps matter as much as the medicine itself.
Doctors usually prescribe calcium acetate for folks with kidney problems, especially those going through dialysis. This medicine helps keep phosphate levels in check, so bones and blood vessels don’t get overloaded. I’ve seen family go through these treatments—the diet changes, the constant juggling of pills. Keeping phosphate down matters quite a bit to prevent complications.
Nobody likes to talk much about the small aches and annoyances until they hit home. With calcium acetate, the gut feels it most. Upset stomach shows up for many, making meals turn into a guessing game. Nausea, sometimes even vomiting, leads a lot of patients to wonder if their lunch or the medicine is to blame. Constipation or diarrhea—one or the other—can stick around, making bathroom habits unpredictable.
Dry mouth is another thing some complain about, and it tends to sneak into the day. Thirst starts to linger, and swallowing thickens up. It doesn’t sound too scary, but after a few weeks, that small annoyance feels a mile wide. Kids or older adults have an even harder time mentioning it, so the side effects sometimes sit in silence for months.
High calcium levels bring their own troubles. Doctors call it hypercalcemia, and the line between “treating phosphate” and “overloading calcium” gets pretty thin. Folks might feel bone pain, muscle weakness or even confusion. Heart rhythms don’t always stay steady; in rare cases, the beats drift off track. For people who already have heart disease, this risk gets even more real.
A friend of mine, after starting calcium acetate, felt tired and grumpy for weeks. We shrugged it off as kidney issues. Her doctor finally checked her calcium, and sure enough, it was sky-high. That adjustment in her pills changed her whole mood and energy. It’s a good reminder not to brush off new symptoms as just “something about dialysis.”
Some drugs mix poorly with calcium acetate. Certain antibiotics, especially tetracyclines and quinolones, lose their punch. Thyroid medicine also drags when taken too close to calcium. I learned this juggling act while helping a neighbor organize their pill box, spacing out meds and checking with the pharmacy each time someone prescribed something new.
Side effects catch up with those who aren’t talking regularly with their medical team. Keeping a close eye on blood tests, like calcium and phosphate levels, matters a lot more than most realize. Pharmacists help spot medicine clashes, so it’s always worth sharing the full list—not just the ones you think matter.
Eating habits can help, too. Doctors often combine calcium acetate with diet changes—cutting back on foods high in phosphate or the ones that throw off calcium balance. No magic food or pill fixes everything, but paying attention takes a load off the medicine’s shoulders.
Calcium acetate has a real place in kidney care, but it’s not something to leave alone once it’s started. Regular check-ins, asking questions about how you feel, and not hiding odd symptoms make all the difference.
Calcium acetate pops up on the prescription list, mostly for folks dealing with chronic kidney disease or trouble with high phosphate levels. Doctors hand it out because it grabs phosphate in the gut, which stops it from getting into the blood. It’s not some rare or back-shelf remedy—people see this name a lot at dialysis clinics and sometimes even in hospital rooms for those struggling with complicated kidney problems.
Not everyone hears about how this compound interferes with other medicine. Calcium itself loves to get involved, sometimes attaching to other drugs in your stomach and blocking them from doing their job. For example, taking calcium acetate alongside certain antibiotics, especially tetracycline or fluoroquinolone types, can cut how much of those antibiotics actually make it into the bloodstream. That’s worth knowing if someone is fighting off an infection and counting on antibiotics to work fast.
Digoxin, often used for heart problems, can also run into trouble. Mixing digoxin with too much calcium raises the risk of irregular heartbeats. I’ve seen patients get confused about why they suddenly don’t feel right after starting something new, only to find out later it was the silent chemical brawl happening in their gut.
Calcium acetate doesn’t stop at prescription drugs. Even common supplements stir up issues. Anyone taking iron, zinc, or magnesium can end up absorbing less if they swallow them near the time they take their calcium dose. Multivitamins promise a boost but fail to mention how one pill can cancel out the benefits of another.
Pharmacists often catch this during medication reviews. Patients sometimes forget to mention those chewable tablets or daily vitamin packs. It’s not just older adults either—anyone juggling chronic disease meds gets caught in this web. Studies, like those published in American Journal of Kidney Diseases, have flagged a rising trend in hidden interactions between mineral binders and supplements, costing people both money and results.
Even meal timing changes things. Calcium in dairy or fortified foods can tip the balance, particularly if someone chases their morning pill with a big bowl of cereal and milk. For people already watching lab results like hawks, these surprises make it so much harder to keep things steady.
Dietitians often step in to help patients choose the right time for each dose, sometimes suggesting spacing out calcium acetate and other pills by a couple of hours. This isn’t just nitpicking—it’s the sort of detail that turns a staggered schedule into better health or fewer problems down the line.
Talking directly with a healthcare provider—doctor, pharmacist, or dietitian—can sort out confusion. Every prescription fill could come with a reminder about timing and cross-checking all current meds and supplements. An updated medication list in a pocket or phone proves more powerful than people realize, cutting down the risk of these surprise interactions.
For anyone who manages a complex routine of pills, separating doses by time, tracking what goes into the body, and staying open about new symptoms makes a difference. Systems like electronic health records and pill organizers have made this a more manageable chore. Technology or not, nothing replaces a real conversation with someone who knows the ins and outs of how bodies and medicines work together.
Calcium acetate finds its way into a lot of medicine cabinets, especially for people living with chronic kidney disease. It tackles phosphate levels, keeping them in check when kidneys can't do the work. A lot of folks see it as just another prescription on the counter. The trouble is, taking it is not for everyone. Personal experience tells me that not every pill works for every person. It always helps to ask hard questions before adding any new medication to a daily routine.
Folks with naturally high calcium in their blood have to be careful. Doctors call this "hypercalcemia." This condition often goes unnoticed until blood tests flag it. Some reasons for high calcium include parathyroid trouble or certain cancers. My grandmother ran into this after a long bout of feeling tired and weak; her doctor warned against any extra calcium. Adding calcium acetate in these situations can tip the scales, making things worse. Muscle pain, kidney stones, stomach upset, or even irregular heartbeats can follow. That’s a risk best avoided. Bloodwork guides smart decisions, not guesswork.
Chronic kidney disease sits at the center of calcium acetate use, but not every kidney patient benefits. Some folks have a mix of heart rhythm issues or very advanced disease. Too much calcium may mess with the delicate balance that keeps hearts beating normally. People with a history of irregular heartbeats need to think twice. In my circle, a friend with kidney issues got extra calcium through another supplement; he began having palpitations that put him in the hospital. The link took a sharp doctor to catch. Pills may look harmless, but their effects go deep.
Some people already take high doses of vitamin D—doctors often suggest it to help absorb calcium. Mixing high vitamin D intake with calcium acetate can quickly push calcium too high. Busy clinics sometimes overlook these overlaps. Signs of this overload show up as bone pain, confusion, or even kidney damage. Looking at everything on the prescription list helps, but talking openly with a healthcare provider matters more. Reviewing supplements counts, too, not just prescriptions. Facts from the National Kidney Foundation back this approach: monitoring both calcium and vitamin D together offers a real line of defense against unforeseen side effects.
Calcium acetate rarely gets prescribed for children or those expecting a baby. Safety in these groups isn’t well known. Doctors take extra care because a growing child or unborn baby responds differently to medications. Pregnancy changes metabolism and can shift mineral balances, too. When I worked with pediatric care teams, we always called in the pharmacy for double checks before approving anything like this. If the science isn’t clear, it’s better to stay on the safe side until new research fills in the blanks.
Family medical history shapes decisions here. Bone diseases, inherited kidney disorders, parathyroid problems—all these influence whether calcium acetate fits safely. Doctors rely on detailed patient histories for a reason: these stories often hold the clues that blood tests won't reveal. Honest conversation with a healthcare provider—sharing past diagnoses and current supplements—makes for safer choices all around. The medical community agrees: tailoring each decision to the patient, instead of following a chart, prevents trouble down the road.
| Names | |
| Preferred IUPAC name | Calcium diacetate |
| Other names |
Acetic acid, calcium salt
Calcium diacetate Calcium ethanoate |
| Pronunciation | /ˈkæl.si.əm ˈæs.ɪ.teɪt/ |
| Identifiers | |
| CAS Number | 62-54-4 |
| 3D model (JSmol) | ``` data 3 Calcium acetate O=C([O-])C.[Ca+2].O=C([O-])C ``` |
| Beilstein Reference | 505657 |
| ChEBI | CHEBI:31344 |
| ChEMBL | CHEMBL1201502 |
| ChemSpider | 53758 |
| DrugBank | DB00364 |
| ECHA InfoCard | 03c5c1b7-a12c-4916-8d6b-44cbee3a1561 |
| EC Number | 208-140-2 |
| Gmelin Reference | 40206 |
| KEGG | C02418 |
| MeSH | D000077185 |
| PubChem CID | 305 |
| RTECS number | FF8050000 |
| UNII | 5FB73Q837J |
| UN number | UN1748 |
| CompTox Dashboard (EPA) | DTXSID2020137 |
| Properties | |
| Chemical formula | Ca(C2H3O2)2 |
| Molar mass | 158.17 g/mol |
| Appearance | White, hygroscopic powder |
| Odor | Odorless |
| Density | 1.5 g/cm³ |
| Solubility in water | slightly soluble |
| log P | -3.3 |
| Vapor pressure | Negligible |
| Acidity (pKa) | 12.6 |
| Basicity (pKb) | 5.3 |
| Magnetic susceptibility (χ) | −35.0×10⁻⁶ cm³/mol |
| Refractive index (nD) | 1.422 |
| Viscosity | 5 mPa·s (10% solution) |
| Dipole moment | 0 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | 157.8 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -1137.6 kJ/mol |
| Std enthalpy of combustion (ΔcH⦵298) | -1796.9 kJ/mol |
| Pharmacology | |
| ATC code | A12AA04 |
| Hazards | |
| Main hazards | May cause respiratory irritation. May cause eye, skin, and respiratory tract irritation. |
| GHS labelling | GHS07, GHS Hazard Statement: H319 |
| Pictograms | GHS07 |
| Signal word | Warning |
| Hazard statements | Hazard statements: H319 Causes serious eye irritation. |
| Precautionary statements | Precautionary statements: P233, P234, P264, P270, P301+P312, P305+P351+P338, P330, P337+P313, P403+P404, P501 |
| NFPA 704 (fire diamond) | 2-0-0 |
| Autoignition temperature | > 790 °C (1454 °F; 1063 K) |
| Lethal dose or concentration | LD50 oral rat 4,270 mg/kg |
| LD50 (median dose) | LD50 (median dose): Oral-rat LD50: 4,260 mg/kg |
| NIOSH | N113 |
| PEL (Permissible) | Not established |
| REL (Recommended) | 1300 mg/day |
| Related compounds | |
| Related compounds |
Calcium carbonate
Calcium chloride Acetic acid Magnesium acetate Sodium acetate |